Upper GI Endoscopy
An upper GI endoscopy lets your healthcare provider look at the first part of your gastrointestinal (GI) tract with an endoscope. This is a thin tube with a camera and a light at the end. The endoscope is put into your throat and advanced down the esophagus. The esophagus, stomach, and the first part of the small intestine (the duodenum) make up the upper GI tract.
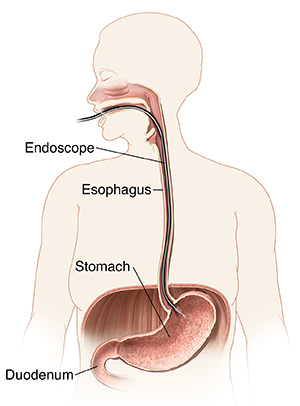 |
| During endoscopy, a long, flexible tube is used to view the inside of your upper GI tract. |
Before the test
Follow these and any other instructions you're given before your endoscopy. If you don’t follow the healthcare provider’s instructions carefully, the test may need to be canceled or done over:
-
Follow any directions you're given for not eating or drinking before your test. In some cases, you may be able to take medicines with sips of water until 2 hours before the test. Talk with your provider about this.
-
Bring your X-rays and any other test results you have.
-
Because you will be sedated, arrange for a trusted adult to drive you home after the exam.
-
Tell your provider before the exam if you're taking any medicines. This includes any over-the-counter and prescription medicines, vitamins, herbs, and supplements. Some medicines may be adjusted or stopped before the test. Don't stop any medicine unless directed by your provider.
-
Tell your provider if you have any health problems.
The procedure
Here is what to expect:
-
You will lie on the endoscopy table. People often lie on their left side.
-
You will be placed on a heart monitor and given oxygen.
-
Your throat may be numbed with a spray or gargle. You're given medicine through an IV (intravenous) line placed in your hand or arm. These medicines will help you relax and stay comfortable. You may be awake and drowsy or asleep during the test.
-
The healthcare provider will put the endoscope in your mouth and down your esophagus. This tube is thinner than most pieces of food that you swallow. It won't affect your breathing. The medicine helps keep you from gagging.
-
Air is put into your GI tract to expand it. It can make you burp.
-
During the procedure, the healthcare provider can take tissue samples (biopsies) and remove abnormalities, such as small bumps or growths (polyps). The provider can also treat abnormalities using tiny tools placed through the endoscope. You won't feel this.
-
The endoscope sends images of your upper GI tract to a video screen. If you're awake, you may be able to look at the images.
After the procedure
-
After the procedure is done, you'll rest and be monitored for a time (anywhere from 1 hour after the test to overnight, depending on complexity).
-
An adult must drive you home. You should not drive for the remainder of the day or longer if recommended by your healthcare provider.
-
You may be tired the rest of the day.
-
You may feel gassy or crampy for a few hours. You may have a sore throat. This should improve in 1 or 2 days.
-
Do not eat or drink until the numbing medicine has worn off and you are able to swallow without gagging.
-
Start with a "soft diet" as advised by your healthcare team. A soft diet is food that is well tolerated and easy to swallow and digest. Examples include soup, eggs, pudding, and applesauce. Advance your diet to other items if you are tolerating soft foods well and once the soreness improves. To stay hydrated, drink plenty of fluids unless your healthcare team has told you not to.
Risks
Risks of upper endoscopy include:
-
A reaction to the sedative, including breathing or heart problems
-
A perforation (or hole) in the lining of your upper GI tract
-
Bleeding (usually minor if it occurs)
When to call your healthcare provider
Call your healthcare provider right away if you have:
-
A firm or distended belly
-
Trouble swallowing or severe sore throat
-
Crunching sensation under the skin around the neck
-
Black or tarry stools, or blood in your stool
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Pain in your belly that is bad or doesn't go away
-
Upset stomach and vomiting, or vomiting blood or black materials
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Melinda Murray Ratini DO
Online Medical Reviewer:
Robyn Zercher FNP
Date Last Reviewed:
3/1/2024
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.